
By Marnie Werner, Vice President of Research
Rural families face a number of headwinds when it comes to accessing mental health services for their children. The heart of the problem, the lack of mental health workers in rural areas, is complex, and the solutions aren’t cheap: higher pay for mental health workers, more opportunities for training in rural areas, more financial support for newly graduated providers while they work to get licensed.
Unfortunately, solving these problems may take years. (For a larger discussion of the mental health workforce, read our report on the mental health workforce shortage here). But the trend in children’s mental health problems needs addressing now, especially in rural areas, where services and even information are harder to come by.
The need
We already know there’s a problem, and it can be hard to even understand the magnitude of it. But while the growth in the number of cases of children needing help with their mental health is disturbing, what is startling is how fast that growth has happened. In December 2023, the Minnesota Department of Health released the results of the 2022 Minnesota Student Survey, a survey of fifth-, eighth-, ninth-, and eleventh-graders conducted every three years. The survey results showed that unhealthy behaviors like tobacco and alcohol use were down, but there was “an unprecedented amount of long-term mental health, behavioral or emotional problems.” Jan Malcolm, Minnesota Commissioner of Health at the time, stated about the report’s findings, “It is clear that this is a crisis.”[1]
The data showed a continuing rise in mental health issues, especially among girls. In 2019, 35% of girls taking the survey and 18% of boys said they had been dealing with long-term mental, emotional and behavioral health issues (“long-term” meaning more than six months). In 2022, the girls’ figure had jumped to 45% while the boys’ number rose to 20%.[2]
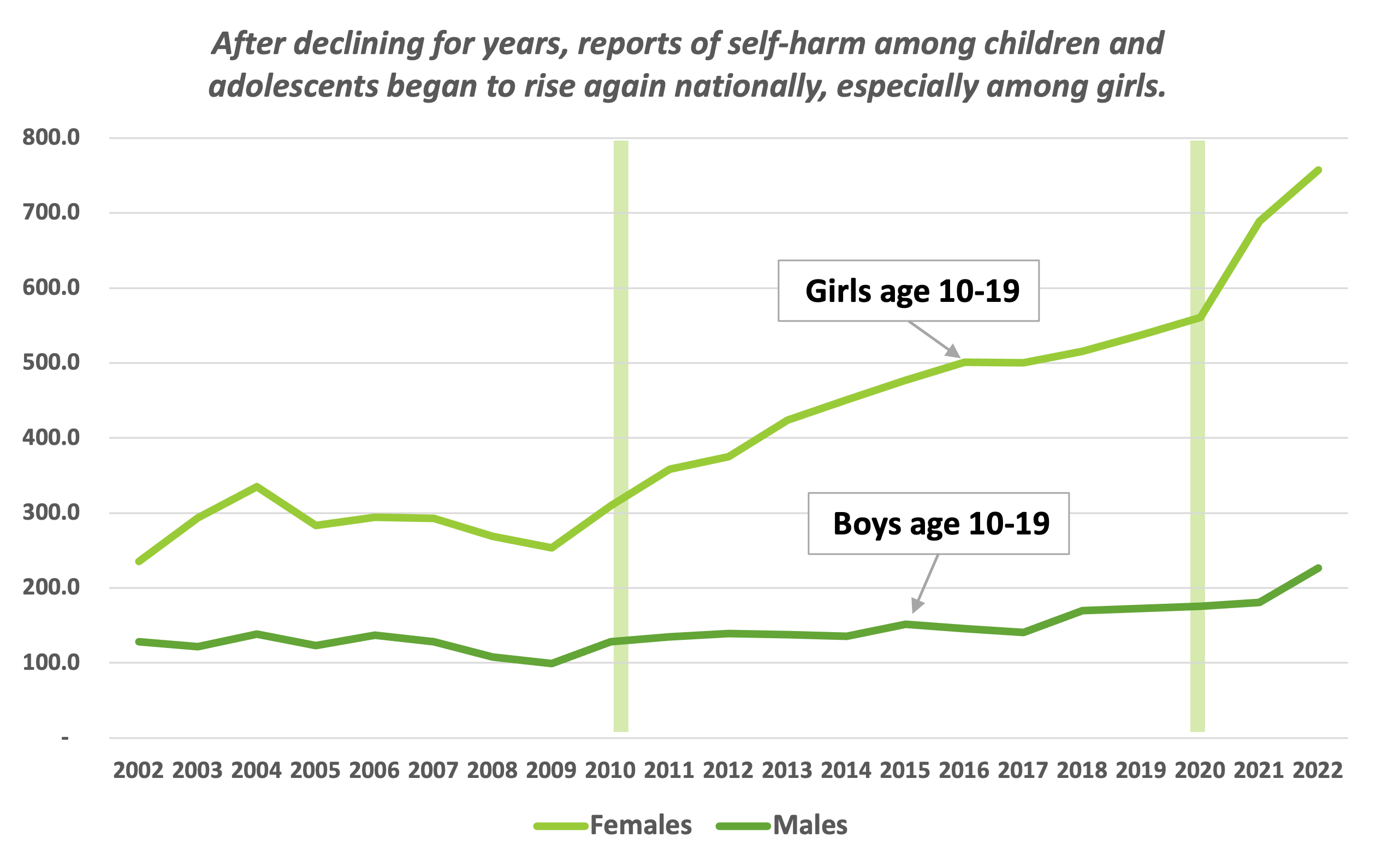
Figure 1: Cases of self-harm among U.S. adolescents ages 10-19, per 100,000, 2002-2022. Source: Centers for Disease Control.
Nationwide, rates of suicide and thoughts of suicide skyrocketed to the point where in 2023, the American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association together declared “a National State of Emergency in Children’s Mental Health.”[3]
The pandemic didn’t help. Isolation and loneliness have always been big factors affecting the state of a person’s mental health. Therefore, while rates of depression and anxiety were going up before the pandemic, COVID appeared to aggravate the situation.
In addition, the growing number of studies demonstrating a connection between social media and poor mental health have had parents and policymakers across the country rethinking children’s access to social media and smart phones.
“I think, honestly, social media had a lot to do with it,” “it” being kids’ declining mental health before the pandemic, said Sue Abderholden, executive director of the National Alliance on Mental Illness–Minnesota. “Then COVID hit, and that really hit kids hard.”
Getting on the continuum of care
At the same time this plight of poor mental health has been striking kids, the United States has been struggling to improve access to mental health services. As far back as 2003, a report to the Minnesota state legislature stated that “Minnesota’s mental health system is a system in crisis.”[4]
Access to mental health services does tend to be more difficult in rural areas. A study from Maine found that when demographics, risk factors, and other characteristics were controlled for, rural children were less likely to be diagnosed with a psychiatric illness other than ADHD and were less likely to receive counseling.[5]
“Distance has always been a concern in rural areas,” says Deborah Cavitt, manager of advocacy and education at the Minnesota Association for Children’s Mental Health. Over the years she has heard stories of families that have needed to drive long distances, sometimes from the Arrowhead down to southern Minnesota, simply because that’s where the provider the family’s insurance will accept is located.
Being screened and diagnosed is the important first step in getting help, since a diagnosis opens the door to the array of services available to a child. This array, known as the continuum of care, provides people with help that ranges in intensity from counseling and play therapy to an inpatient stay at a hospital. Not recognizing and addressing mental health problems early allows them to build, and therefore, the earlier a child with mental health issues can enter this continuum, the sooner their problems can be addressed, hopefully keeping little problems from turning into big problems.
“There is a strong and growing body of evidence demonstrating positive outcomes when youth with mental illnesses have access to a well-coordinated continuum of mental health services and supports,” states a 2019 study by Wilder Research.[6]
The question for parents, though, is how to know if their kids need help, and if they do, how to get them on the continuum of care. But the continuum of care is fragmented, especially for children. When a child has a full-on crisis, parents especially in rural areas, often have no place to go but the emergency room at the closest hospital.
Using the emergency room presents a problem, however, in that many hospitals, including rural ones, are not always equipped to treat children having a mental health crisis. Using the emergency room also sets in motion rules and policies that can keep kids trapped there. Once a child has been prescribed a form of treatment, the hospital can’t discharge that child until they can move on to that treatment. If the child was prescribed treatment at an in-patient facility, they could be waiting a long time until a bed becomes available, or the parents simply take them home.
Creating more beds would help children who are already in crisis, of course, but “more beds” is not about furniture—it is about the trained workers needed to serve the children who occupy those beds, and now we’re back to the issue of workforce.
Like many professions across America, health care and mental health care are facing a wave of people retiring, while at the same time seeing a shortage of people entering colleges and universities and coming out the other side with the credentials to practice. We discussed this issue in our 2023 research on the mental health workforce shortage and the accompanying webinar. Because of the number of people retiring every year combined with the amount of time it takes to train a mental health care provider and the difficulty in attracting people to practice in rural areas, it will take years to fill out the workforce needed, if that can be accomplished ever.
Focusing only on beds for in-patient treatment also ignores the fact that a child doesn’t suddenly go into crisis for no reason. Mental illnesses develop over a lifetime, and most start early, with approximately 50% developing by age 14 and 75% by age 24.[7]
What do we do?
The key is catching kids early through prevention and early intervention, greatly reducing the demand for beds in the long run because children are being treated early, hopefully while the illness is still small, which improves their chances of having a happy, productive life.
But given the shortage of mental health care providers in rural areas, the long waiting lists to see a provider, and other problems like stigma and transportation, what are rural parents supposed to do in the meantime?
Fortunately, we found three opportunities parents can take advantage of right now with resources we already have in rural areas.
Opportunity #1: Educate yourself.
As the Minnesota Student Survey showed, the percentage of kids dealing with episodes of mental illness has grown drastically in the last several years, and poor mental health doesn’t just go away on its own, especially for children. With brains that are still developing, most kids and teens don’t have the capacity to “pull themselves together” or express just what’s making them anxious or depressed.
That’s why it’s critical for parents to understand the basics about mental health, especially in children. Knowledge can help alleviate fears over what might just be kids being kids or help parents know when it could be something more.
The first thing to know: 988
The first thing for parents to know and understand is that 988, the Suicide and Crisis Lifeline, is there to answer questions. In 2022, the National Suicide Prevention Lifeline phone number was replaced by 988, a number that is open to anyone looking for more information on mental health, how to find services, or even wondering what to do for their child when they’re not even sure something is wrong. When you think something is wrong but you don’t know what, you can call, text or chat about it via 988 with someone in Minnesota.[8] You can read more about 988 here and here.
For more information
If you want to know more about mental health and mental illnesses in children but you’re not ready to talk to someone about your child, the MN Department of Health website has many links to resources and information on mental health, as does the National Alliance on Mental Illness–Minnesota. NAMI-MN has numerous booklets and links to information on everything from what it looks like when someone is in crisis to how to navigate the mental health system.
Another resource is the Minnesota Association for Children’s Mental Health, which helps families find providers, navigate the system, and find guidance through certified family peer specialists, people who have been through the mental health system with their own children and are now trained to help other families, says Cavitt.
One example at the local level is Brown County Human Services, which has a web page on children’s mental health that goes over the signs and symptoms, what a diagnostic assessment is, and who parents can call with their concerns.
Mental health versus mental illness
The next thing to keep in mind is that “mental health” is not the same as “mental illness” any more than “physical health” equals “physical illness.” Mental health is simply the state of a person’s emotional, psychological, and social well-being, just like physical health is about how your body feels and behaves.
Everyone has good days and bad days, and so do children. A person’s mental health affects how that person thinks, feels, acts, and how well they handle stress, relate to others, and make choices. Good mental health allows people to cope with life’s stresses, realize their goals to the best of their abilities, and contribute to their community.[9]
About 20% or so of Minnesota children and youth ages 0-17 have diagnosed mental illnesses. What causes mental illness in a particular child is complicated and can involve everything from neurological issues with the brain to family life and traumatic events the child experiences, even diet and sleep (see Table 1). These experiences, known as risk factors, are cumulative, which means the more risk factors a child faces, the more likely they are to develop a mental illness.[10]
Table 1: Both risk factors and protective factors can shape a child’s mental health for the rest of their life.
|
Level |
Risk factors |
Protective factors |
|
Individual Characteristics |
Difficult temperament; inflexibility; poor concentration; low self-esteem; poor social skills; shyness; rebelliousness; insecure attachment; withdrawal. |
Academic achievement; intellectual development; emotional self-regulation; coping skills; problem-solving skills; engagement/connections in school with peers, in athletics, employment, religion, or culture. |
|
Family characteristics |
Depression; marital/family conflict; poor parenting; substance use; child abuse; maltreatment; or unemployment. |
Family provides structure, limits, rules, monitoring, and predictability. The child has supportive relationships with family members and clear expectations of behavior and values. |
|
School/Community characteristics |
Peer rejection; community/school violence; poverty; poor academic achievement; community-level stressful or traumatic events; drug use in community or at school. |
Presence of mentors and support for development of skills and interests; opportunities for engagement within school and community; positive norms; clear expectations of behavior and safety. |
Results First. “Children’s Mental Health Inventory and Benefit-Cost Analysis.” MN Management & Budget, January 2019.
Prevention, promotion, and early intervention
But just as risk factors are cumulative, so are protective factors, positive aspects of children’s lives that help make them resilient in the face of life’s trials. Kids living with more challenges may be at greater risk for mental illness, but early intervention can offset those risk factors with protective factors like a stable and predictable family environment; healthy, supportive relationships; mentors; and skills like emotional self-regulation, coping, and problem-solving.[11]
Again, early intervention is important. According to the American Association of Pediatrics, most youth having suicidal ideas or who are planning or have attempted suicide have one or more pre-existing mental health disorders.[12] The sooner the illness can be identified, the sooner it can be treated before it escalates.
Along with early intervention, there are promotion and prevention. Anna Lynn is the mental health promotion coordinator at the Minnesota Department of Health, where she focuses on advancing a public health approach to mental well-being through policy and programming designed to help the whole community. Promoting good mental health involves figuring out what would help everyone to be well, regardless of whether a person has an illness or not, says Lynn. At the same time, prevention targets people—including children—who are already facing risk factors.
“There’s a whole set of things that we know can promote well-being,” says Lynn. With kids especially, it’s building healthy, positive relationships with other kids and with adults. Social and emotional skills are also something children need to learn, and even adults are not always great at identifying their emotions. “We all know sad-mad-glad,” says Lynn, “but we don’t always know how or why it’s important to identify how we’re feeling so that we can actually address it and not bury it.”
Opportunity #2: Integrating mental health into primary care.
Primary care is increasingly becoming a first step in accessing mental health care for children. According to the MN Department of Health’s Office of Rural Health and Primary Care, a large percentage of both urban and rural physicians already provide some aspect of mental health services (89% rural, 83% urban) in the absence of other options.[13]
The first thing a family doctor should be able to do is check whether what’s concerning parents about their child is some kind of physical issue. After that, most MDs can treat non-complex mental illnesses like generalized anxiety disorder and depression, but more complex cases require someone trained and licensed in mental health.
According to the Centers for Disease Control, however, while nine out of ten children see their primary healthcare provider regularly, in 2018 only one in three pediatricians reported that they had enough training to diagnose and treat children with mental disorders.[14] Given the rising demand and shortage of workers, health care systems are starting to adopt “behavioral health integration,” an idea that has been around for a while but is gaining new traction.
Behavioral health integration comes in two types:
- A more basic service called general behavioral health integration, or BHI, that can potentially be delivered by a physician alone.[15]
- A psychiatric collaborative care model (CoCM), which involves a team of primary care and mental health providers focused on the one patient.[16]
Dr. Charles Lewis, a child and adolescent psychiatrist and assistant professor in the Department of Psychiatry and Behavioral Sciences at the University of Minnesota Medical School, is involved in one form of the team approach. He meets regularly online with case managers from ten southern Minnesota counties supported by the South Central Community Based Initiative to have an in-depth discussion about their child and teenage clients. The county staff approached the medical school to ask if there was a way members of the psychiatry department could provide consultations for kids in these rural counties, where wait times to see a mental health provider can be very long.
“We talk about the kinds of care that they [the kids] have had already and what additional options might be helpful for them, and then as a team we try to brainstorm ideas for how to overcome some of the barriers they have in accessing care,” says Lewis.
Sanford Health, which operates clinics and hospitals in western Minnesota, North and South Dakota, Iowa, and Montana, has also committed to behavioral health integration. In 1990, Dr. Jeff Leichter became the first behavioral health professional integrated into a Sanford primary care clinic, at its clinic in Detroit Lakes. In 2012, he was asked to head up a large-scale expansion of the program through a grant. Today, Sanford has mental health providers available—in person or virtually—in nearly all its primary care clinics.
Placing these “integrated health therapists,” or IHTs, in regular primary care clinics makes access to mental health screenings and services easier, and it recognizes the impact that mental issues like stress and depression can have on a person’s physical health, and vice versa. A key part of this plan is the “warm handoff.”
“So, if you came in, and let’s say you have diabetes or hypertension, and your doctor decides that maybe you have some lifestyle issues or stress issues going on that might be contributing to your health concerns,” Leichter says, “rather than saying, ‘Hey, here’s a referral to go see a psychologist up in another town seven weeks from now,’ they would do a warm handoff, and literally, the therapist would see you that day in real time in that same visit and do an assessment and perhaps offer some treatment to you.”
Meeting the therapist right away creates an immediate connection, making it more likely that the patient—or the patient’s parents in the case of children—will follow up on future appointments.[17]
Making BHI work in real-world settings may require changes to the way healthcare in the U.S. is done, including changing the way healthcare workers are reimbursed and the culture of health service delivery.[18] For instance, for a mental health professional to submit a charge to the insurance provider for their time, “there has to be a diagnosis of a mental health condition,” Leichter says. Sometimes, though, a person may be in genuine distress, but the IHT isn’t able to make a specific diagnosis. The patient still needs help, but it is not a charge that can be reimbursed. The hope, though, is that if the patient can get their needs or stress addressed earlier on, ultimately this will lead to fewer emergency room visits, unneeded admissions, etc., “which is a win-win for everybody.”
Opportunity #3: School-linked mental health services.
After the pandemic ended and things were getting back to normal at Montevideo Public Schools, Superintendent Wade McKittrick noticed that something still seemed wrong.
“We recognized that the mental health concerns coming out of the shutdown were significant,” said McKittrick. “We were seeing behaviors that we hadn’t really seen before. It wasn’t so much that there were more, but the ones that we were seeing were more significant.”
Through conversations with his schools’ social workers, McKittrick started to recognize themes around mental health: kids couldn’t regulate their emotions and couldn’t cope with stress.
“There was just the perception that there was a lot of untreated mental health issues across the district,” McKittrick said.
When they added it up, the social workers guesstimated that there were around 100 kids who had mental health concerns that were not being addressed.
“That number alarmed me,” McKittrick said.
Across the state and the nation and around the world, teachers, principals and superintendents are noticing the same thing: the mental health of a lot of kids had deteriorated during the pandemic, and it’s playing out at school. It’s not necessarily that more kids are having problems, but that the symptoms of poor mental health that kids were already experiencing got worse, including for those kids whose issues may have been under the radar.
Once McKittrick and the social workers arrived at their number, he invited every local mental health care provider to a conversation. They all recognized the problem as well, but they felt handcuffed, they told him, like there was only so much they could do.
So McKittrick offered them a proposal: they could have free space in the district’s schools and start seeing—and treating—kids right there. The providers started signing up.
One of the most promising developments in mental health care for rural children, school-linked mental health services are a collaboration between school districts and local mental health service providers that puts providers right where they can see and treat children in a familiar place, their school.
Addressing mental health services in schools isn’t exactly new. Schools have had counselors, advisors and social workers for decades. The difference now is that children can get a fuller array of mental health services, including psychotherapy and Children’s Therapeutic Services and Supports (CTSS), a package of mental health treatments and services that are covered by Medicaid and most insurance plans.
School-linked mental health services are huge for rural Minnesota, says Sue Abderholden, because it addresses the biggest barriers to getting mental health services to kids: parents needing to take time off work, transportation issues, and long waits for appointments.
As we discussed in our report from early 2024, fear of what other people will think if they find out someone is being treated for a mental illness—or if their child is—keeps many people away. Parents in particular worry that they’ll be seen as bad parents if their child needs help.
Having services in the school goes a long way toward eliminating that fear because the therapy staff are very good at finding ways to get kids to them without being singled out, says Brittany Sutherland, a mental health professional with North Homes Children and Family Services who oversees the school-based services in Deer River, Remer, and Hill City in north central Minnesota. Many children simply have a set hour during a set day of the week when, instead of having a study hall, they meet with their therapist.
“We can do a lot of planning to help kids feel more comfortable and a little under the radar, you might say, if they do feel nervous and anxious about not wanting people to know,” Sutherland says.
For parents who work during the day, finding time to drive a child to an appointment can be difficult to impossible, especially for rural parents because of the long distances that may be involved. In addition, kids are often prescribed a set number of weeks where they need to see the therapist.
“It’s hard for parents to take that time off,” says Abderholden. The parent must leave work to pick up their child, drive to the provider’s office, which could be in a neighboring city or county, then drive back. It could be three hours by the time the child is back at school. And if the child needs multiple weeks of therapy? “Many employers won’t go for that.”
Perhaps the biggest barrier eliminated or at least reduced is the long wait time to see a provider. Getting a child assessed can be as easy as talking to their teacher.
North Homes provides services in almost fifty schools across northern Minnesota, from Bemidji to Cloquet to Chisholm, plus White Bear Lake and Mahtomedi in the Twin Cities area. North Homes provides individual psychotherapy and CTSS, plus crisis assistance for any child, client or non-client, who may have a crisis during the school day, says Sutherland.
Having their staff in the schools has made delivery of services more seamless and integrated, especially since North Homes staff are seen as part of the school community rather than outsiders. McKittrick is trying to do the same thing in the Montevideo schools, where even though the providers are not members of staff, they’re seen that way, building better relationships between them and kids.
The North Homes counselors also provide training for teachers and school staff, showing what to watch for in kids and strategies to help them. Teachers are familiar with their kids, says Sutherland, so they can tell when someone is just having a bad day or when it’s something else. Changes in their normal behavior, outbursts, talking about pain, or talking about one particular thing a lot more than normal are all signs that something may be wrong, says Sutherland.
One challenge that comes with providing services in schools is keeping lines of communication with the family open. Because the parents don’t see the therapist every session, it can be a challenge to keep parents engaged in their child’s treatment.
“When you bring your child to the outpatient clinic, most parents are walking their child in and checking in with the therapist for five or ten minutes, then you’re sitting outside of the session. I do think that piece gets missed when you’re working in a school and you really don’t see the parent, except maybe once a year at their [child’s] annual assessment,” says Sutherland. For that reason, North Home’s staff use their cell phones to keep building that relationship with parents through texts, emails, and phone calls.
Schools can also be not just a place to receive mental health care but a hub for social services in general. North Homes works closely with the Deer River Schools’ community support coordinator, who helps families with tasks like going to the food pantry, getting to dental or vision appointments, or picking up medications, valuable services for families without transportation who live far from town.
The South Central Service Cooperative in North Mankato does something similar, providing two navigators to the school districts the cooperative serves. These navigators work directly with families to help them access and navigate the complexities of the mental health system and to build relationships with both families and school staff to facilitate communication and coordination of care for students, says Beth Winterfeldt, one of SCSC’s navigators.
Their services are paid for by the child’s health insurance, whether that is private or public (Medicaid, Medicare, MNCare). However, not all health insurance covers all services. If a child is uninsured or underinsured, North Homes has access to funds from the state’s School-Linked Behavioral Health grant, which helps cover co-pays, deductibles, and other costs.
These insurance payments and state grant funds don’t go to schools, they go directly to the mental health care providers, “which is good, because, honestly, we shouldn’t expect schools to be treating mental illness,” says Abderholden. “They should be supporting students and collaborating with the mental health professionals, but they shouldn’t be doing the treating. Parents want a fire wall between education and mental health records. We’re strong advocates for [school-linked mental health services], because we think it works.”
Conclusion
The shortage of mental health services, the long wait times for appointments, and the number of children being treated in emergency rooms are well documented. It all has to do with a shortage of workers in the field. But while various solutions are being developed to increase the number of people in the mental healthcare field, the process will be slow—it takes time to educate a person—and recruitment and retention in rural areas will be constant hurdles to overcome. In the meantime, the rate at which children are reporting mental health issues and the suicide rate among kids and adolescents are at alarming levels.
Right now, there are three opportunities to break down the barriers between kids and the help they need:
- Education for parents on just what mental illness is and is not, especially in children, and the importance of prevention and early intervention;
- Integrating behavioral healthcare into primary care and using other collaborative models; and
- Offering mental health services in schools. These options, while not perfect fixes, could help parents recognize if their child has a problem and help shorten the time a child has to wait to get help.
In the current situation, time is of the essence: mental illnesses do not go away on their own and often only get worse with time. Getting help sooner rather than later is the key to helping children grow into happier, healthier adults.
References
American Medical Association. “Behavioral Health Integration Compendium,” 2024. https://www.ama-assn.org/system/files/bhi-compendium.pdf.
American Psychiatric Association. “APA Behavioral Health Integration Fact Sheet,” June 2022.
Anderson, Kayla N. “Emergency Department Visits Involving Mental Health Conditions, Suicide-Related Behaviors, and Drug Overdoses Among Adolescents — United States, January 2019–February 2023.” MMWR. Morbidity and Mortality Weekly Report 72 (2023).
Arakelyan, Mary, Jennifer A. Emond, and JoAnna K. Leyenaar. “Suicide and Self-Harm in Youth Presenting to a US Rural Hospital During COVID-19.” Hospital Pediatrics 12, no. 10 (September 27, 2022): e336–42.
Bailey, Leisa, Grace Wagstaff, and Diane Little. “Bringing Behavioral Health Into Your Practice Through a Psychiatric Collaborative Care Program.” Aafp.Org, 2019.
Berg-Weger, Marla, Thomas Cudjoe, and Yingying Lyu. “Addressing the Impact of COVID-19 on Social Isolation and Loneliness.” National Academies of Science, July 2024.
Berkel, Jessie van. “Study Proposes Reimbursement Rate Fix for Minnesota’s Broken Mental Health System.” Star Tribune, January 24, 2024.
Board on Health Care Services, Health and Medicine Division, and National Academies of Sciences, Engineering, and Medicine. Exploring Strategies to Improve Access to Behavioral Health Care Services Through Medicare and Medicaid: Proceedings of a Workshop-in Brief. Edited by Udara Perera and Joe Alper. Washington, D.C.: National Academies Press, 2024.
Bogucki, Olivia E., Angela B. Mattson, William B. Leasure, Summer L. Berg, Hannah L. Mulholland, and Craig N. Sawchuk. “Adaptations of an Integrated Behavioral Health Program During COVID-19.” Cognitive and Behavioral Practice 28, no. 4 (November 2021): 481–91.
Bommersbach, Tanner J., Mark Olfson, and Taeho Greg Rhee. “National Trends in Emergency Department Visits for Suicide Attempts and Intentional Self-Harm.” American Journal of Psychiatry, June 4, 2024, appi.ajp.20230397.
Campo, John V., Rose Geist, and David J. Kolko. “Integration of Pediatric Behavioral Health Services in Primary Care: Improving Access and Outcomes with Collaborative Care.” Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 63, no. 7 (July 2018): 432–38.
Centers for Disease Control and Prevention. “About Mental Health,” May 20, 2024.
———. “Data and Statistics on Children’s Mental Health.” Centers for Disease Control and Prevention, June 3, 2022.
———. “Help Children in Rural Communities Thrive.” Centers for Disease Control and Prevention, June 15, 2020.
———. “Mental Health Care, Children and Behavioral Health Integration.” Centers for Disease Control and Prevention, October 18, 2018.
———. “Public Health Strategies for Rural Child Mental Health: Policy Brief,” Centers for Disease Control and Prevention. May 15, 2024.
———. “Children’s Mental Health,” Centers for Disease Control and Prevention. April 27, 2023.
Centers for Medicare and Medicaid Services. “Behavioral Health Integration Services,” May 2023.
“Children’s Mental Health Services.” MN Department of Human Services, January 2018.
Clary, Emily, and Ann Boerth. “2017 Collaborative Report Summary.” MN Department of Human Services, June 8, 2021.
“COE: Prevalence of Mental Health Services Provided by Public Schools and Limitations in Schools’ Efforts to Provide Mental Health Services,” National Center for Education Statistics, 2022.
Cohen, D. J., B. A. Balasubramanian, M. Davis, J. Hall, R. Gunn, K. C. Stange, L. A. Green, et al. “Understanding Care Integration from the Ground Up: Five Organizing Constructs That Shape Integrated Practices.” The Journal of the American Board of Family Medicine 28, no. Supplement 1 (September 1, 2015): S7–20.
Committee on the Impact of Social Media on Adolescent Health, Board on Population Health and Public Health Practice, Health and Medicine Division, and National Academies of Sciences, Engineering, and Medicine. Social Media and Adolescent Health. Edited by Sandro Galea, Gillian J. Buckley, and Alexis Wojtowicz. Washington, D.C.: National Academies Press, 2024.
Cutler, Gretchen J., Kelly R. Bergmann, Stephanie K. Doupnik, Jennifer A. Hoffmann, Mark I. Neuman, Jonathan Rodean, Alicia L. Zagel, and Bonnie T. Zima. “Pediatric Mental Health Emergency Department Visits and Access to Inpatient Care: A Crisis Worsened by the COVID-19 Pandemic.” Academic Pediatrics 22, no. 6 (August 2022): 889–91.
Cutler, Gretchen J., Jonathan Rodean, Bonnie T. Zima, Stephanie K. Doupnik, Alicia L. Zagel, Kelly R. Bergmann, Jennifer A. Hoffmann, and Mark I. Neuman. “Trends in Pediatric Emergency Department Visits for Mental Health Conditions and Disposition by Presence of a Psychiatric Unit.” Academic Pediatrics 19, no. 8 (2019): 948–55.
Davis, Danielle, and Loredana Santo. “Emergency Department Visits Related to Mental Health Disorders Among Children and Adolescents: United States, 2018–2021.” National Center for Health Statistics (U.S.), October 12, 2023.
Dillon, Kristin, Miamoua Vang, and Nathan Hierlmaier. “Transfer and Discharge Delays for Behavioral Health Patients at Minnesota Hospitals.” MN Dept of Health, July 15, 2024.
Evans, Garret, Heidi Radunovich, Michelle Cornette, Brenda Wiens, and Antara Roy. “Implementation and Utilization Characteristics of a Rural, School-Linked Mental Health Program: Journal of Child & Family Studies.” Journal of Child & Family Studies 17, no. 1 (February 2008): 84–97.
Ferris, Melanie. “Children’s Intensive Mental Health Services Study.” Wilder Research, 2019.
Fritsma, Teri, Carrie Henning-Smith, Jacqueline L. Gauer, Faizel Khan, Mark E. Rosenberg, Kirby Clark, Elizabeth Sopdie, Angela Sechler, Michael A. Sundberg, and Andrew P. J. Olson. “Factors Associated With Health Care Professionals’ Choice to Practice in Rural Minnesota.” JAMA Network Open 6, no. 5 (May 4, 2023): e2310332.
“From the Editor: Integrating Behavioral Health Into Primary Care,” Family Practice Management, May/June 2021.
Garcia-Navarro, Lulu. “Robert Putnam Knows Why You’re Lonely.” The New York Times, July 13, 2024, sec. Magazine.
Haidt, Jonathan. The Anxious Generation: How the Great Rewiring of Childhood Is Causing an Epidemic of Mental Illness. New York: Penguin Press, 2024.
Hoffmann, Jennifer A., Camille P. Carter, Cody S. Olsen, David Ashby, Kamali L. Bouvay, Susan J. Duffy, James M. Chamberlain, et al. “Pediatric Mental Health Emergency Department Visits from 2017 to 2022: A Multicenter Study.” Academic Emergency Medicine, April 2, 2024, acem.14910.
Hua, Liwei L., Janet Lee, Maria H. Rahmandar, Eric J. Sigel, Committee on Adolescence and Council on Injury, Violence, and Poison Prevention. “Suicide and Suicide Risk in Adolescents.” Pediatrics 153, no. 1 (January 1, 2024): e2023064800.
Jones, Anne C., and Kaitlin R. Lilienthal. “Integrating Behavioral Health and Primary Care: Turning a Duet into a Trio.” Annals of Family Medicine 21, no. 2 (2023): 185–87.
Krass, Polina, Evan Dalton, Stephanie K. Doupnik, and Jeremy Esposito. “US Pediatric Emergency Department Visits for Mental Health Conditions During the COVID-19 Pandemic.” JAMA Network Open 4, no. 4 (April 30, 2021): e218533.
Maeng, Daniel D., Ellen Poleshuck, Tziporah Rosenberg, Amie Kulak, Thomas Mahoney, George Nasra, Hochang B. Lee, and Yue Li. “Primary Care Behavioral Health Integration and Care Utilization: Implications for Patient Outcome and Healthcare Resource Use.” Journal of General Internal Medicine 37, no. 11 (August 2022): 2691–97.
Minnesota Department of Health. “2022 Minnesota Student Survey Results Released,” December 23, 2022.
———. “Minnesota Mental Health Professional Shortage Areas,” 2016.
———. “Minnesota Pediatric Mental Health Access Program.”———. “Rural Health Care in Minnesota.” Minnesota Department of Health, 2024.
———. “Recommendations on Strengthening Mental Health Care in Rural Minnesota 2021.” June 3, 2021.
NAMI Minnesota. “Keeping Families Together: A Guide to the Children’s Mental Health System.” namimn.org, April 2024.
———. “Navigating a Mental Health Crisis.” namimn.org, 2018.
Pickner, Wyatt J., Susan E. Puumala, Kaushal R. Chaudhary, Katherine M. Burgess, Nathaniel R. Payne, and Anupam B. Kharbanda. “Emergency Department Utilization for Mental Health in American Indian Children.” The Journal of Pediatrics 174 (July 2016): 226-231.e3.
Results First. “Children’s Mental Health Inventory and Benefit-Cost Analysis.” MN Management & Budget, January 2019.
SAMHSA. “Minnesota 2022 Uniform Reporting System Mental Health Data Results.” samhsa.org, 2022.
Schickedanz, Adam, and Neal Halfon. “Evolving Roles for Health Care in Supporting Healthy Child Development.” Future of Children 30, no. 2 (Fall 2020): 143–64.
Searcey van Vulpen, Kimberly, Amy Habegar, and Teresa Simmons. “Rural School-Based Mental Health Services: Parent Perceptions of Needs and Barriers: Children & Schools.” Children & Schools 40, no. 2 (April 2018): 104–11.
“Study Describes More Severe Pediatric Mental Health Crises during Pandemic | CIDRAP,” April 2, 2024.
“The Institute of Medicine’s Continuum of Care.” Strategic Prevention Technical Assistance Center, n.d.
Trangle, Michael. “State Advisory Council on Mental Health Subcommittee on Children’s Mental Health,” 2022.
“Using Medicaid to Address Young People’s Mental Health Needs in School Settings,” April 10, 2024.
Vivek H. Murthy. “Protecting Youth Mental Health | The U.S. Surgeon General’s Advisory,” Office of the Surgeon General, 2021.
Werner, Marnie. “Mental Health Services in Greater Minnesota,” Center for Rural Policy and Development, ruralmn.org, May 25, 2017.
Wilger, Susan. “Special Considerations for Mental Health Services in Rural Schools.” Substance Abuse and Mental Health Services Administration, n.d.
[1] https://www.health.state.mn.us/news/pressrel/2022/stsurvey122322.html
[2] https://public.education.mn.gov/MDEAnalytics/DataTopic.jsp?TOPICID=242
[3] Hua et al., 2024, p. 1.
[4] “Mental Health: A System in Crisis,” Minnesota Office of Ombudsman for Mental Health and Developmental Disabilities, 2003.
[5] Anderson, Nathaniel J, Samantha J Neuwirth, Jennifer D Lenardson Mhs, and David Hartley. “Patterns of Care for Rural and Urban Children with Mental Health Problems,” n.d., ii.
[6] Ferris, Melanie. “Children’s Intensive Mental Health Services Study.” Wilder Research, 2019,
- 35.
[7] Campo, John V., Rose Geist, and David J. Kolko. “Integration of Pediatric Behavioral Health Services in Primary Care: Improving Access and Outcomes with Collaborative Care.” Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 63, no. 7 (July 2018): 432–38. https://doi.org/10.1177/0706743717751668.
[8] Calls to 988 are routed based on the area code of the caller’s phone number. If you live in Minnesota but have a phone with an area code outside Minnesota, your call will be routed to that state. However, anyone you reach will be able to help you.
[9] Centers for Disease Control, “About Mental Health,” May 20, 2024.
[10] Results First. “Children’s Mental Health Inventory and Benefit-Cost Analysis.” MN Management & Budget, January 2019, p. 12.
[11] Results First. “Children’s Mental Health Inventory and Benefit-Cost Analysis.” MN Management & Budget, January 2019.
[12] Hua, Liwei L., Janet Lee, Maria H. Rahmandar, Eric J. Sigel, Committee on Adolescence and Council on Injury, Violence, and Poison Prevention. “Suicide and Suicide Risk in Adolescents.” Pediatrics 153, no. 1 (January 1, 2024).
[13] “Rural Health Care in Minnesota.” Minnesota Department of Health, 2024.
[14] “Mental Health Care, Children and Behavioral Health Integration | CDC.” Centers for Disease Control and Prevention, October 18, 2018.
[15] Campo, John V., Rose Geist, and David J. Kolko. “Integration of Pediatric Behavioral Health Services in Primary Care: Improving Access and Outcomes with Collaborative Care.” Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 63, no. 7 (July 2018): 432–38.
[16] Bailey, Leisa, Grace Wagstaff, and Diane Little. “Bringing Behavioral Health Into Your Practice Through a Psychiatric Collaborative Care Program.” aafp.org, 2019, p. 11-12.
[17] Bailey et al., 2019, p. 12.
[18] Campo et al., 2018, p. 432.
